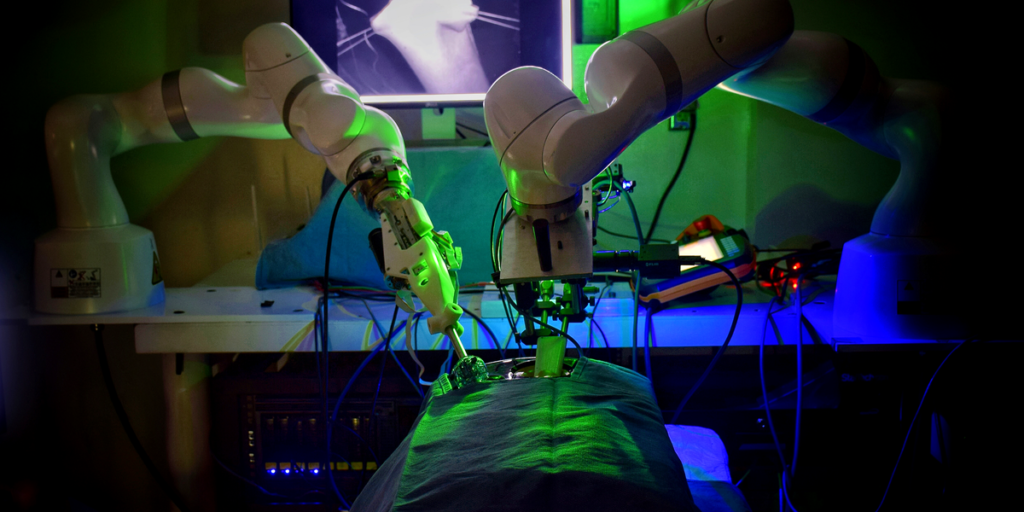
Right here’s a scene from the not-too-distant future. In a vibrant, high-tech operating room, a glossy robotic arm stands poised subsequent to the working desk. The autonomous robotic received’t function utterly alone, however it should help within the upcoming process, performing key duties independently with enhanced precision and diminished danger.
Its affected person is one among more than 150,000 patients identified with colon cancer within the United States alone every year. The one healing remedy is to take away the diseased a part of the colon—ideally in a minimally invasive laparoscopic process, carried out with surgical tools and a skinny digicam inserted by small incisions. However the surgery tends to be difficult. The surgeon’s abilities, expertise, and method are essentially the most important factors influencing surgical outcomes and complications, which happen in as much as 16 percent of cases. These problems can diminish the affected person’s high quality of life and improve the chance of loss of life. The hope is that an autonomous surgical robotic will enhance these odds.
See the Good Tissue Autonomous Robotic (STAR) in motion on this video demonstrating how the system laparoscopically sutures a chunk of small gut.
Throughout surgical procedure, this robotic will carry out duties that require the utmost accuracy. The surgeon will first management its motions by hand to take away the cancerous tissue, then supervise the robotic’s movement because it independently sews the remaining wholesome colon again collectively. Utilizing a number of types of imaging and real-time surgical planning, the robotic will place every sew with submillimeter precision, a feat not potential with human arms. In consequence, the ensuing suture line will likely be stronger and extra uniform, making it much less more likely to leak, a harmful complication that may happen when the connection doesn’t heal correctly.
Whereas autonomous robots aren’t but getting used to function on individuals in the way in which we’ve simply described, we now have the instruments able to this futuristic type of surgical procedure, with extra autonomy on the way in which. Our crew, centered round coauthor Axel Krieger’s robotics lab at Johns Hopkins University, in Baltimore, is devoted to creating robots that may carry out complicated, repetitive duties extra persistently and precisely than the best surgeons. Earlier than too lengthy, a affected person might anticipate to listen to a brand new model of the acquainted greeting: “The robotic will see you now.”
Robotic-assisted surgical procedure dates back to 1985, when a crew of surgeons at Lengthy Seashore Memorial Medical Heart, Calif., used an tailored industrial robot arm to information a needle right into a mind for a biopsy. Though the process went nicely, Westinghouse, the robotic’s producer, halted additional surgical procedures. The corporate argued that as a result of the robotic was designed for industrial functions, it lacked essential security options. Regardless of this hitch, surgical robots continued to evolve. In 1994, U.S. regulators accredited the primary surgical robotic: the Automated Endoscopic System for Optimum Positioning (AESOP), a voice-controlled robotic arm for laparoscopic digicam positioning. The 12 months 2000 noticed the introduction of the da Vinci robot, a teleoperated system that allows surgeons to have fantastic management over tiny devices.
The primary model of STAR sutured a chunk of small gut pulled up by an incision.Ryan Decker
Surgeons are a cautious bunch, and so had been initially sluggish to undertake the expertise. In 2012, lower than 2 % of surgical procedures in america concerned robots, however by 2018, that number rose to about 15 percent. Surgeons discovered that robots supplied clear benefits for sure procedures, such because the removing of the prostate gland—right this moment, more than 90 percent of such procedures in america are robot-assisted. However the advantages for a lot of different surgical procedures stay unsure. The robots are costly, and the human surgeons who use them require specialised coaching, main some consultants to query the general utility of robotic help in surgical procedures.
Nonetheless, autonomous robotic techniques, which might deal with discrete duties on their very own, may probably show higher efficiency with much less human coaching required. Surgical procedure requires spectacular precision, regular arms, and a excessive diploma of medical experience. Studying easy methods to safely carry out specialised procedures takes years of rigorous coaching, and there’s little or no room for human error. With autonomous robotic techniques, the excessive demand for security and consistency throughout surgical procedure may extra simply be met. These robots may handle routine duties, forestall errors, and probably carry out full operations with little human enter.
The necessity for innovation is evident: The variety of surgeons world wide is shortly lowering, whereas the quantity of people that want surgical procedure continues to extend. A 2024 report by the Affiliation of American Medical Faculties predicted a U.S. scarcity of as much as 19,900 surgeons by the 12 months 2036. These robots current a approach for hundreds of thousands of individuals to achieve entry to high-quality surgical procedure. So why aren’t autonomous surgical procedures being carried out but?
Sometimes, once we consider robots within the office, we think about them finishing up manufacturing facility duties, like sorting packages or assembling vehicles. Robots have excelled in such environments, with their managed situations and the comparatively small quantity of variation in duties. For instance, in an auto manufacturing facility, robots within the assembly line set up the very same components in the very same place for each automotive. However the complexity of surgical procedures—characterised by dynamic interactions with mushy tissues, blood vessels, and organs—doesn’t simply translate to robotic automation. In contrast to managed manufacturing facility settings, every surgical situation presents sudden conditions that require making choices in actual time. That is additionally why we don’t but see robots in our day-to-day lives; the world round us is filled with surprises that require adapting on the fly.
Growing robots able to navigating the intricacies of the human physique is a formidable problem that requires refined mechanical design, modern imaging strategies, and most lately, superior artificial-intelligence algorithms. These algorithms should be able to processing real-time knowledge to be able to adapt to the unpredictable setting of the human physique.
STAR: An Autonomous Surgical Bot
2016 marked a serious milestone for our discipline: One among our crew’s robotic techniques performed the primary autonomous soft-tissue surgical procedure in a reside animal. Known as the Smart Tissue Autonomous Robot, or STAR, it sewed collectively tissue within the small gut of a pig utilizing a commercially out there robot arm whereas supervised by a human surgeon. The robotic moved independently between suturing places alongside the tissue edge and waited for the surgeon’s approval earlier than autonomously putting the stitches. This management technique, known as supervised autonomy, is usually used to ensure surgeons keep engaged when automating a essential job.
STAR’s suturing was the primary time a robotic had demonstrated autonomous surgical efficiency that was objectively higher than the usual of care: In contrast with the efficiency of human surgeons, STAR achieved extra constant suture spacing, which creates a stronger and extra sturdy suture line. And a stronger sew line can stand up to larger pressures from inside the gut with out leaking, in contrast with sutures finished by the guide laparoscopic method. We think about this a groundbreaking achievement, as such leaks are essentially the most dreaded complication for sufferers receiving any sort of gastrointestinal surgical procedure. As much as 20 percent of sufferers receiving surgical procedure to reconnect the colon develop a leak, which might trigger life-threatening infections and should require extra surgical procedure.
 The 2016 STAR system sutures the small gut with a single robotic arm. Behind the robotic, a display reveals near-infrared and 3D imaging facet by facet. Ryan Decker
The 2016 STAR system sutures the small gut with a single robotic arm. Behind the robotic, a display reveals near-infrared and 3D imaging facet by facet. Ryan Decker
Earlier than this 2016 surgical procedure, autonomous soft-tissue surgical procedure was thought-about a fantasy of science fiction. As a result of mushy tissue continually shifts and contorts, the surgical discipline adjustments every time the tissue is touched, and it’s not possible to make use of presurgical imaging to information a robotic’s movement. We had additionally been stymied by the state of surgical imaging. The very best cameras that had been appropriate with surgical scopes—the lengthy, skinny tubes used to view inside surgical procedures—lacked the quantifiable depth info that autonomous robots want for navigation.
Essential improvements in surgical instruments and imaging made the STAR robotic a hit. As an illustration, the system sutured with a curved needle, simplifying the movement wanted to go a needle by tissue. Moreover, a brand new design allowed a single robotic arm to each information the needle and management the suture pressure, so there was no danger of instruments colliding within the surgical discipline.
However crucial innovation that made STAR potential was using a novel dual-camera system that enabled real-time monitoring of the gut throughout surgical procedure. The primary digicam supplied colour pictures and quantifiable three-dimensional details about the surgical discipline. Utilizing this info, the system created surgical plans by imaging the intestinal tissue and figuring out the optimum places for the stitches to yield the specified suture spacing. However on the time, the imaging fee of the system was restricted to 5 frames per second—not quick sufficient for real-time utility.
To unravel this limitation, we launched a second, near-infrared digicam that took about 20 images per second to trace the positions of near-infrared markers positioned on the goal tissue. When the place of a given marker moved an excessive amount of from one body to the following, the system would pause and replace the surgical plan based mostly on knowledge from the slower digicam, which produced three-dimensional pictures. This technique enabled STAR to trace the soft-tissue deformations in two-dimensional house in actual time, updating the three-dimensional surgical plan solely when tissue motion jeopardized its success.
This version of STAR may place a suture on the right location on the primary attempt just a little greater than half the time. In observe, this meant that the STAR system wanted a human to maneuver the suture needle—after it had already pierced the pores and skin—as soon as each 2.37 stitches. That fee was practically on par with how often human surgeons need to right the needle place when manually controlling a robotic: as soon as each 2.27 stitches. The variety of stitches utilized per needle adjustment is a essential metric for quantifying how a lot collateral tissue is broken throughout a surgical procedure. Basically, the less instances tissue is pierced throughout surgical procedure (which corresponds to the next variety of sutures per adjustment), the higher the surgical outcomes for the affected person.
For its time, the STAR system was a revolutionary achievement. Nonetheless, its dimension and restricted dexterity hindered docs’ enthusiasm, and it was by no means used on a human affected person. STAR’s imaging system was a lot larger than the cameras and endoscopes utilized in laparoscopic surgical procedures, so it may carry out intestinal suturing solely by an open surgical method wherein the gut is pulled up by a pores and skin incision. To switch STAR for laparoscopic surgical procedures, we wanted one other spherical of innovation in surgical imaging and planning.
Enhancing STAR’s Surgical Autonomy
In 2020 (outcomes printed in 2022), the following technology of STAR set one other document on the earth of soft-tissue surgical procedure: the primary autonomous laparoscopic surgery in a live animal (once more, intestinal surgical procedure in a pig). The system featured a brand new endoscope that generates three-dimensional pictures of the surgical scene in actual time by illuminating tissue with patterns of sunshine and measuring how the patterns are distorted. What’s extra, the endoscope’s dimensions had been sufficiently small to permit the digicam to suit inside the opening used for the laparoscopic process.

 The autonomy afforded by the 2020 STAR system permits surgeons to take a step again from the surgical discipline [top]. Axel Krieger [bottom] takes an in depth take a look at STAR’s suturing. Max Aguilera Hellweg
The autonomy afforded by the 2020 STAR system permits surgeons to take a step again from the surgical discipline [top]. Axel Krieger [bottom] takes an in depth take a look at STAR’s suturing. Max Aguilera Hellweg
Adapting STAR for a laparoscopic strategy affected each a part of the system. As an illustration, these procedures happen inside restricted workspace within the affected person’s stomach, so we had so as to add a second robotic arm to take care of the right pressure within the suturing thread—all whereas avoiding collisions with the suturing arm. To assist STAR autonomously manipulate thread and to maintain the suture from tangling with accomplished stitches, we added a second joint to the robotic’s surgical instruments, which enabled wristlike motions.
Now that the gut was to be sutured laparoscopically, the tissue needed to be held in place with non permanent sutures in order that STAR’s endoscope may visualize it—a step generally finished within the nonrobotic equal of this process. However by anchoring the gut to the belly wall, the tissue would transfer with every breath of the animal. To compensate for this motion, we used machine learning to detect and measure the motions attributable to every breath, then direct the robotic to the proper suture location. In these procedures, STAR generated choices for the surgical plan earlier than the primary sew, detected and compensated for movement inside the stomach, and accomplished most suturing motions within the surgical plan with out surgeon enter. This management technique, known as job autonomy, is a elementary step towards the total surgical autonomy we envision for future techniques.
Whereas the unique STAR’s technique of tissue detection nonetheless relied on using near-infrared markers, latest developments in deep learning have enabled autonomous tissue monitoring with out these markers. Machine studying strategies in image processing additionally shrank the endoscope to 10 millimeters in diameter and enabled simultaneous three-dimensional imaging and tissue monitoring in actual time, whereas sustaining the identical accuracy of STAR’s earlier cameras.
All these advances enabled STAR to make fantastic changes throughout an operation, which have diminished the variety of corrective actions by the surgeon. In observe, this new STAR system can autonomously full 5.88 stitches earlier than a surgeon wants to regulate the needle place—a a lot better final result than what a surgeon can obtain when working a robotic manually for the complete process, guiding the needle by each sew. By comparability, when human surgeons carry out laparoscopic surgical procedure with none robotic help, they alter their needle place after virtually each sew.
AI and machine studying strategies will possible proceed to play a outstanding function as researchers push the boundaries of what surgical jobs may be accomplished utilizing job automation. Finally, these strategies may result in a extra full sort of automation that has eluded surgical robots—to this point.
The Way forward for Robotic Surgical procedure
With every technical advance, autonomous surgical robots inch nearer to the working room. However to make these robots extra usable in scientific settings, we’ll have to equip the machines with the instruments to see, hear, and maneuver extra like a human. Robots can use computer vision to interpret visible knowledge, natural-language processing to grasp spoken directions, and superior motor management for exact actions. Integrating these techniques will imply {that a} surgeon can verbally instruct the robotic to “grasp the tissue on the left”or “tie a knot right here,” as an example. In conventional robotic surgical procedure techniques, in contrast, every motion must be described utilizing complicated mathematical equations.
 Specialised imaging allows STAR’s laparoscopic suturing. The purple dots right here present the system’s proposed suture places. Hamed Saeidi
Specialised imaging allows STAR’s laparoscopic suturing. The purple dots right here present the system’s proposed suture places. Hamed Saeidi
To construct such robots, we’ll want general-purpose robotic controllers able to studying from huge datasets of surgical procedures. These controllers will observe skilled surgeons throughout their coaching and discover ways to adapt to unpredictable conditions, resembling soft-tissue deformation throughout surgical procedure. In contrast to the consoles utilized in right this moment’s robotic surgical procedures, which give human surgeons direct management, this future robotic controller willuse AI to autonomously handle the robotic’s actions and decision-making throughout surgical duties, decreasing the necessity for fixed human enter—whereas maintaining the robotic beneath a surgeon’s supervision.
Surgical robots working on human sufferers will collect an unlimited quantity of knowledge and, finally, the robotic techniques can prepare on that knowledge to discover ways to deal with duties they weren’t explicitly taught. As a result of these robots function in managed environments and carry out repetitive duties, they’ll constantly study from new knowledge, bettering their algorithms. The problem, nevertheless, is in gathering this knowledge throughout numerous platforms, as medical data is delicate and certain by strict privateness rules. For robots to achieve their full potential, we’ll want in depth collaboration throughout hospitals, universities, and industries to coach these intelligent machines.
As autonomous robots make their approach into the scientific world, we’ll face more and more complicated questions on accountability when one thing goes unsuitable. The surgeon is historically accountable for all elements of the affected person’s care, but when a robotic acts independently, it’s unclear whether or not liability would fall on the surgeon, the producer of the robotic {hardware}, or the builders of the software program. If a robotic’s misinterpretation of knowledge causes a surgical error, for instance, is the surgeon at fault for not intervening, or does the blame lie with the expertise suppliers? Clear pointers and rules will likely be important to navigate these situations and be certain that affected person security stays the highest precedence. As these applied sciences turn out to be extra prevalent, it’s additionally necessary that sufferers be absolutely knowledgeable about using autonomous systems, together with the potential advantages and the related dangers.
A situation wherein sufferers are routinely greeted by a surgeon and an autonomous robotic assistant is not a distant risk, because of the imaging and management applied sciences being developed right this moment. And when sufferers start to profit from these developments, autonomous robots within the working room received’t simply be a risk however a brand new customary in drugs.
From Your Web site Articles
Associated Articles Across the Internet